After an injury, a healing program is initiated in epithelial cells. They tightly coordinate themselves so that they do not divide too much or too little. Dr. Anne-Kathrin Classen from the Cluster of Excellence CIBSS - Centre for Integrative Biological Signalling Studies is investigating why this process sometimes goes awry. Using the model organism of the fruit fly Drosophila, the cell biologist is investigating which signalling pathways control tissue repair. At some point this knowledge could lead to better treatment for chronic wounds.
Despite seemingly good planning, cells in injured tissues sometimes become uncoordinated. In tissue healing programs, this could lead to delayed tissue repair and chronic wounds. Cell biologist Anne-Kathrin Classen in the CIBSS Cluster of Excellence is investigating the molecular mechanisms behind normal and impaired healing and regeneration of tissues. The research group leader at the Center for Biological Systems Analysis (ZBSA) at the University of Freiburg is investigating how epithelial cells behave after tissue injuries. How does their healing program start? “It is also important to know how the cells return to their normal state,” says Classen who works with the model organism of the fruit fly Drosophila. Is it possible that new knowledge will eventually prevent chronic wounds? Classen also hopes to find out how cellular signalling pathways of tissue regeneration and tumor growth are connected.
Injuries stress the tissue
Injuries mean stress for the tissue. “The cells sense that something has been damaged,” explains Classen. First they process this information, then they communicate with surrounding cells and finally with the rest of the organism. “The cells coordinate which signalling pathways should be activated.” If everything goes well, the process leads to a healed and healthy tissue. For this, the cells must neither divide too much nor too little. According to the cell biologist, perfect healing is not always achieved: “There are situations in which the tissue does not find the right balance.”
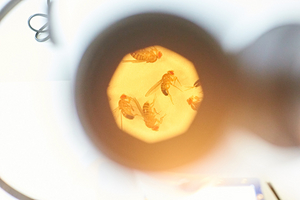
Classen, who studied cell and developmental biology in Manchester and Amsterdam, explores tissue regeneration using the Drosophila model. With her 10-person team, she prepares the 0.3 millimeter small imaginal discs from the one millimeter larvae of the fruit fly: “This is one cell layer with up to 40,000 epithelial cells each.” Epithelial cells form the outer boundary layer of multicellular organisms, for instance the uppermost cell layer of skin and mucous membranes in humans.
In order to investigate tissue repair, the researchers minimally wound the Drosophila larvae, either mechanically with small needles, or genetically, by manipulating epithelial cells in such a way that they produce excess amounts of the signalling factor TNF-α and thereby die. This leads to signals that start tissue repair: cells begin to proliferate. But not always, as is the case with impaired wound healing. “Our system serves as a model for this,” explains Classen. Her research group has shown that when wound healing is impaired, cell proliferation does not function properly because epithelial cells suffer from prolonged stress and cannot effectively coordinate the signalling pathways that promote healing.
Footprints on the DNA
The transcription factors AP-1, STAT and YAP play important roles in this process. Like other transcription factors, they switch their target genes on or off by binding to specific stretches of DNA in the genome. “We suspect that AP-1, STAT and YAP have significant roles in the tissue repair program,” says the cell biologist. She hopes to identify the target genes of these transcription factors. Do these genes ensure appropriate cell proliferation in the normal healing program?
Her research group couples genes for fluorescent proteins to the binding sites of STAT, AP-1 and YAP. When the transcription factors switch on one of their target genes, a fluorescent protein is produced. “This visual readout enables us to observe the activity of STAT, AP-1 and YAP in tissue under the microscope,” says the researcher. Alternatively, she can modify STAT, AP-1 and YAP themselves so that they leave a chemical footprint at their binding sites when they associate with DNA. “We isolate these binding sites and can characterize all them by sequencing.” With these and other methods, Classen hopes to unravel the transcription program that starts when injuries occur. How do cells initiate this program? How can they exit this program during normal wound healing, and why is this impaired during abnormal healing? “How do the epithelial cells that bring about normal or impaired tissue repair differ?” she asks.