N Engl J Med. 2020;382(3):294-296.
Extracorporeal photopheresis for colitis induced by checkpoint-inhibitor therapy
Combined immune checkpoint-inhibitor therapy with anti-CTLA4 and anti-PD-1 antibodies is an efficient first-line treatment for malignant melanoma. However, approximately 50% of the patients develop serious immune-related adverse events (irAE)1,2. Autoimmune colitis occurs in 20% of the cases and can become corticosteroid-refractory3. We here report a patient suffering from ipilimumab/nivolumab-induced colitis, refractory to multiple immunosuppressive drugs, who achieved a complete response after extracorporeal photopheresis (ECP) coinciding with an expansion of immuno-regulatory natural killer (NK) cells.A 29-year old male patient was treated with ipilimumab and nivolumab for metastatic melanoma. After two doses, the patient developed dermatitis, thyroiditis, hepatitis and colitis. Colitis was diagnosed based on macroscopic mucosal ulcerations and intraepithelial apoptosis and crypt loss identified in the biopsy (Fig. 1a,b). While dermatitis, thyroiditis and hepatitis resolved after stopping ipilimumab/nivolumab and corticosteroid treatment, the patient experienced three colitis episodes within the next 20 weeks (CTC-AE II-III°). These were treated with corticosteroids (in total 23 weeks prior to ECP), infliximab (2 single doses 18 and 15 weeks prior to ECP) and cyclosporine (14 weeks prior to ECP, Fig. 1a and Table S1). Since there was no durable response, the patient received ECP. During the next 8 months, he underwent 2 cycles of ECP on consecutive days every 2-4 weeks. ECP was well tolerated and led to a complete response (Fig. 1a). Immunosuppression was tapered without symptom rebound. Continuous remission of colitis was confirmed by colonoscopy (Fig. 1c). Immune checkpoint-inhibitor treatment was discontinued upon first manifestation of irAE and never resumed.
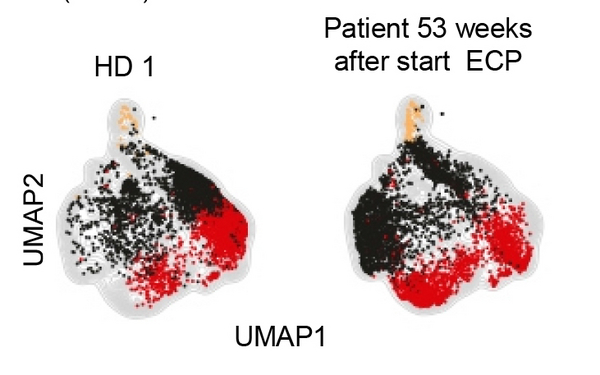
We analyzed the peripheral blood leukocyte compartment at multiple time points before and during ECP treatment. We observed a 4-fold increase in NK cells (Fig. 1d-e, Fig. S1a-j), with an immuno-regulatory phenotype (Fig. 1f,g). Also multiple pro-inflammatory cytokines were lower in the patient compared to age-matched healthy donors (Fig. S2a-e). Supporting the notion that NK cells regulated autoimmunity, adoptive transfer of the patient's NK cells prevented irAE in a murine irAE model triggered by human T cells and anti-PD-1 antibody-treatment in a dose-dependent manner (Fig. 1h and Fig. S3a,b). Control experiments confirmed that morbidity was mediated by the patient-derived T cells (Fig. S4).
ECP is an established therapy for the treatment of graft-versus-host disease (GVHD)4 and leads to an increase of NK cells in GVHD patients5. Data regarding safety and efficacy of ECP for irAE treatment have been lacking so far. This case report implicates that ECP can be an efficient therapy for refractory checkpoint inhibitor-associated colitis through the expansion of a protective NK cell population.