Gearing Up Against Breast Cancer: Unravelling Oncogenic Signalling and the Tumour Microenvironment to Enhance γδ-Based Adoptive Cell Transfer
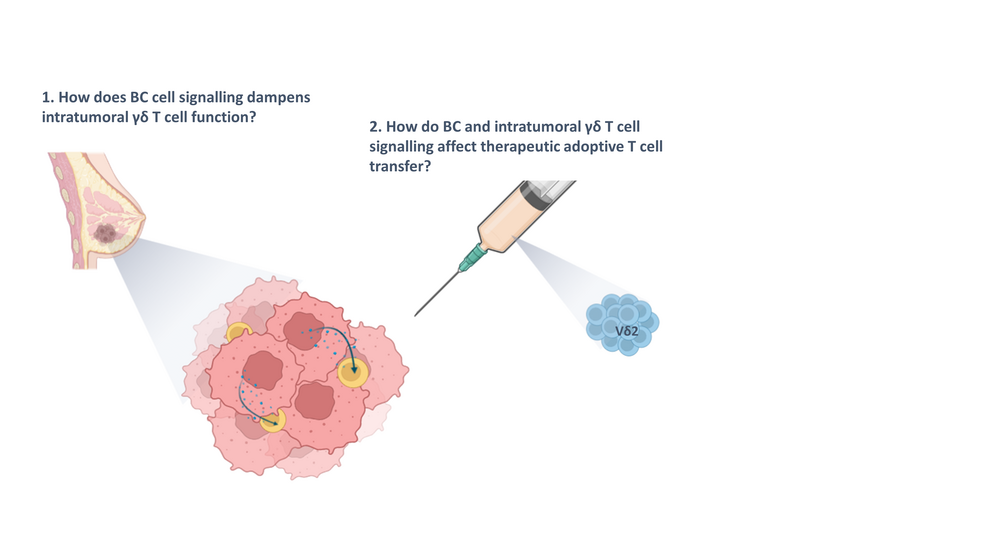
Breast cancer (BC) is the most prevalent and deadliest cancer among women worldwide. γδ T cells, a unique type of T cells positioned at the intersection of innate and adaptive immunity, have shown potential for immunotherapies since their ability to suppress skin cancer was discovered in 2014. This unique T cell population possess antitumour mechanisms resembling both αβ T cells and natural killer (NK) cells, allowing them to quickly eliminate cancer cells independently of MHC class I antigen presentation. The distinct advantage of γδ T cell immunotherapy lies in its HLA-unrestricted nature, which permits the use of cells from healthy donors. Studies have shown that γδ cells from BC patients can be expanded and displayed enhanced cytotoxicity and cytokine release in vitro1. However, the application of γδ T cell immunotherapy in BC treatment is limited to few studies dealing with triple negative breast cancer (TNBC), one molecular subtype, leaving their use against all other subtypes unexplored2–4. My mission is to contribute to the development of improved BC treatments by leveraging my experience with T cell-based immunotherapies as well as my knowledge and interest in breast cancer. I aim to use the CIBSS Launchpad funds to develop an improved 3D model system combining patient-derived cancer cells and cells of the tumour microenvironment (TME) to address how BC cell signalling affects on one hand, γδ T cell-mediated adoptive cell transfer (ACT), and on the other hand, tumour-infiltrating γδ T cells.Additionally, the project will explore γδ T cell signalling will be addressed to address T cell activation and exhaustion upon BC cell encounter.